The rotator cuff consists of four tendons that attach the surrounding muscles to the greater and lesser tuberosity of the shoulder. It serves to keep the ball centered in the socket and is important in motions such as forward elevation, external rotation, and internal rotation. Tears can occur acutely with a fall or other traumatic mechanism, or they can be chronic in nature. Symptoms include anterior or lateral shoulder pain and weakness with arm elevation or abduction. Night pain is common. Chronic tears are more commonly age-related or secondary to impingement. Rotator cuff tears can be partial or full thickness. Full thickness tears can vary in size and number of tendons involved. These types of tears do not heal on their own and can necessitate surgical treatment. A large percentage of tears can be repaired through arthroscopic techniques (as seen in image below). Healing rates and outcomes depend on a number of factors such as tendon tear size, degree of retraction, overall tendon quality, and muscle atrophy. In certain cases, repair techniques can be augmented with allograft tissue to improve the overall biology of healing. A sling is typically needed for 6 weeks post-operatively and a structured physical therapy program is usually started within this post-op time period. Overall recovery from rotator cuff surgery can be up to 6 months and functional improvement can be made for up to 1 year post-operatively.

Watch video of Arthrex Speedbridge repair technique
Treatment of massive irreparable tears can include debridement, tendon transfers, or newer techniques such as superior capsule reconstruction (SCR). SCR utilizes suture anchors to affix a small piece of allograft tissue from the superior aspect of the socket over to lateral greater tuberosity to help maintain the humeral head centered in the socket.
The rotator cuff consists of four tendons that attach the surrounding muscles to the greater and lesser tuberosity of the shoulder. Rotator cuff tendonitis and impingement are commonly seen in adults. The condition usually results from repetitive overuse activities of the shoulder. The subacromial bursa lies between the rotator cuff tendons and the acromion and can initially become inflamed. Spur formation can occur over the anterior and lateral acromion which also contributes to impingement of the rotator cuff tendons. In later stages, the top part of the rotator cuff tendon becomes inflamed or thickened, which is called tendinopathy. Symptoms include pain over the anterior or lateral shoulder with reaching, lifting, or repetitive use. Initial treatment is typically conservative to include anti-inflammatory medications, corticosteroid injection, physical therapy, and activity modification. Surgical treatment may be necessary and includes outpatient arthroscopic debridement of the rotator cuff and subacromial decompression to remove any bony impingement. Overall recovery is usually 6-8 weeks.

The biceps tendon of the shoulder is comprised of a short and long head. The long head is a tendon that runs from the muscle belly, up through the bicipital groove, into the joint attaching to the top part of the glenoid (socket). There can be inflammation or tearing of the tendon anywhere along this path (picture above showing tear of biceps tendon within the joint). Symptoms consist of anterior shoulder pain, popping/snapping, or cramping. In some cases, rupture of the tendon occurs resulting in a popeye deformity. Surgical treatment for biceps tendon pathology can include a tenotomy (which is a release of the tendon at its attachment site on the superior glenoid) or tenodesis (a release of tendon with re-attachment at a different location in the proximal humerus). Recovery can require use of a sling for 4-6 weeks and can be a minimum of three months if a tenodesis is performed.
Stability of the shoulder is achieved through bony and soft tissue constraints. The labrum is a fibrocartilagenous ring that deepens the socket and serves as an attachment site for the glenohumeral ligaments which provide additional static stability to the shoulder. Instability refers to a subluxation (or dislocation) event that can be traumatic or atraumatic in origin. Traumatic dislocations occur when the ball dislocates in an anterior-inferior or posterior direction. These injuries result in a tearing of the labrum and stretching of the glenohumeral ligaments. It can also result in bony damage to the ball or socket. For younger patients in particular, an initial subluxation or dislocation can significantly increase the risk of recurrent instability episodes and further damage to the labrum and articular cartilage of the joint. Surgical treatment involves arthroscopically repairing the labrum and tightening the capsule back to the socket. Patients need a sling for up to 6 weeks to allow for healing. Full recovery can be upwards of 4-6 months.
Watch knotless shoulder labral repair with Arthrex PushLock technique
Shoulder osteoarthritis occurs secondary to loss of articular cartilage of the ball and socket joint. Pain, crepitus (grinding), and stiffness are the most common complaints. Conservative (non-surgical) treatment includes activity modification, non-steroidal anti-inflammatory medications, corticosteroid injections, and a range of motion program. Surgical treatment includes arthroscopic extensive debridement (removal of damaged cartilage), biologic resurfacing procedures, or total shoulder replacement. Total shoulder replacement is the most definitive treatment option in advanced cases. A detailed operative plan can be created using 3D CT scan imaging ordered pre-operatively. The surgery usually requires an overnight hospital stay. It involves a pre-operative nerve block performed by the anesthesia team and the surgery is done under general anesthesia. It includes replacing the arthritic humeral head with a metal ball and resurfacing the socket with a thin polyethylene component. The rotator cuff is always preserved to allow the shoulder to function optimally after surgery. Some implant systems offer a stemless humeral component designed to minimize humeral bone removal (see two images at the end of this section). Augmented glenoid components are also available to address posterior glenoid deficiency in certain patients. Following surgery, patients wear a sling for up to 6 weeks. A structured therapy program is needed after surgery. Full recovery is typically 4-6 months in most patients.
The picture to the left is a pre-operative image demonstrating severe shoulder osteoarthritis. The picture to the right is one following a total shoulder replacement in the same patient.



The acromioclavicular (AC) joint is the joint above the shoulder where the end of the clavicle (collarbone) meets the acromion (top part of the shoulder blade). The joint is stabilized by ligaments and capsule and additionally by strong ligaments between the end of clavicle and corocoid called the coracoclavicular ligaments. Problems of this joint can be acute or chronic. Acute AC joint injuries are called sprains and are usually the result of a direct fall onto the point of the shoulder. Acute AC joint sprains are graded by the severity of injury to the surrounding ligaments. High grade sprains result in deformity of the end of the clavicle because it is no longer stabilized by surrounding ligaments. In these cases, surgical reconstruction is sometimes necessary. Multiple different reconstruction procedures are available, some of which incorporate allograft (cadaver) tissue to rebuild the ligaments. Surgery is typically outpatient, requires use of a sling for 6 weeks, and can be a 4-6 month recovery.
Additional AC joint pathology includes arthritis and osteolysis of the end of the clavicle. Arthritis is where the cartilage begins to wear down and bone spurs begin to form. Pain, crepitus (grinding), and swelling are common. Conservative treatment includes activity modification, anti-inflammatory medications, or a corticosteroid injection. Surgical treatment involves removal of the end of the clavicle and can be done arthroscopically or via open techniques. Overall recovery is usually 6-8 weeks. Osteolysis involves resorption of the subchondral bone of the end of the clavicle and typically presents in a similar fashion to AC joint arthritis. It is commonly seen in weightlifters or laborers who do frequent repetitive overhead activities. Treatment recommendations are similar to AC joint arthritis.
Rotator cuff tear arthropathy refers to a special type of arthritis of the shoulder joint that occurs secondary to a chronic massive rotator cuff tear. A normal functioning rotator cuff keeps the ball of the shoulder centered in the socket. A chronic massive rotator cuff tear allows the ball to migrate superiorly in the socket, altering the biomechanics of the joint and leading to an abnormal wear pattern and eventual arthritis. Symptoms include pain and progressive loss of overhead motion, leading to a pseudoparalytic shoulder in some patients. Surgical treatment depends on the stage of the disease process. For those with weakness and loss of overhead motion, a reverse shoulder replacement can be very effective. The surgery usually requires an overnight hospital stay. It involves a pre-operative nerve block performed by the anesthesia team and the surgery is done under general anesthesia. Following surgery, patients wear a sling for up to 6 weeks. A structured therapy program is needed after surgery. Full recovery is typically 4-6 months in most patients.

Frozen shoulder (or adhesive capsulitis) most commonly occurs in patients in their 40s-60s, females more so than males, and those with endocrine disorders such as type 2 diabetes or thyroid problems. A traumatic event may trigger the condition, although in a large number of cases there is no inciting event. Patients usually present with pain and loss of range of motion. The pain can be severe, especially in the early phases of the disease process. The level of stiffness can vary from patient to patient, but can be very functionally limiting. Conservative treatment includes a corticosteroid injection and a range of motion program, either at home or with a physical therapist. Fortunately, a majority of cases can resolve without the need for surgery, but can take up to 12-18 months. For patients that have persistent stiffness in spite of a therapy program, surgical treatment consists of an arthroscopic lysis of adhesions with manipulation under anesthesia. Overall recovery can by 6-8 weeks.
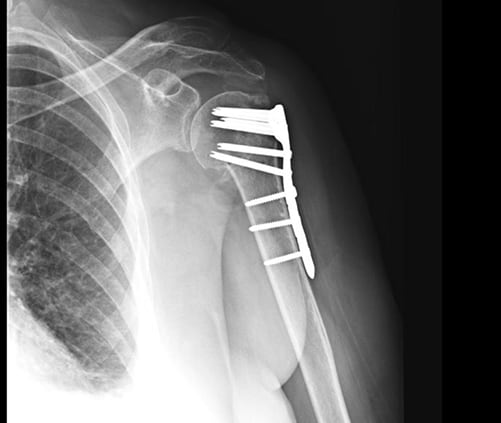
Proximal humerus fractures are a break of the upper part of the arm at the junction of where the humeral head meets the shaft. The proximal humerus consists of four main ‘parts’ that include the head, shaft, greater tuberosity, and lesser tuberosity. The tuberosities are the attachment sites for the 4 rotator cuff tendons. There are multiple variations of this type of injury, which can be classified by the number of parts fractured. Depending on the fracture pattern on x-ray, many can be treated non-operatively in a sling. The bone usually heals over 8-12 weeks. Certain fracture patterns warrant surgical treatment, which can include open reduction internal fixation (ORIF), partial shoulder replacement, or reverse shoulder replacement. The decision is typically based on the fracture pattern, patient age, and overall bone quality.