The anterior cruciate ligament is one of two main central stabilizing ligaments in the knee. It controls anterior tibial translation and rotation. It is estimated that 100,000 to 200,000 ACL injuries occur in the United States each year. Females are at two to six times increased risk of injury compared to males. Injury to this ligament occurs most commonly through a non-contact mechanism in cutting/pivoting sports such as basketball, football, and soccer. Additional injuries are common and include meniscal tears, articular cartilage lesions, and other ligament sprains, most commonly the medial collateral ligament.

Surgical reconstruction is often necessary to restore stability to the knee. The surgery requires use of autograft (patient’s own) or an allograft (cadaveric) tissue source to rebuild the ligament. Autograft tissue is most commonly used and includes the central third of the patellar tendon or quadrupled hamstrings tendon. Allograft tissue is an option in certain cases and depends on patient age, activity level, and patient/surgeon preference. Surgery is typically performed as an arthroscopically-assisted procedure in an outpatient setting. Post-operative physical therapy plays a critical role in recovery. Post-op therapy should also incorporate exercises for the opposite knee to minimize future injury risk to that knee. Full return to play is based on functional testing results with a physical therapist and can range anywhere from 6-12 months. Neuromuscular strengthening/training programs have been established and studied and are now being used to lower index ACL injury rates in athletes.
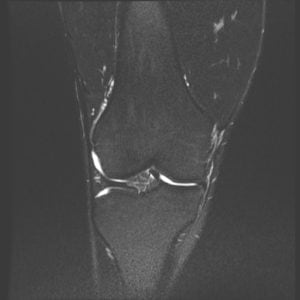
The meniscus is a c-shaped pad of fibrocartilage that acts as a shock absorber between the femur and tibia. There is a medial and lateral meniscus in each knee. A tear of the meniscus may occur in isolation or in conjunction with a ligament injury such as an ACL tear. Meniscal tear patterns can be highly variable among patients and treatment is often based on the tear pattern. Tears may cause symptoms such as pain, locking, catching, or swelling. Surgical treatment includes arthroscopic removal of the torn portion of the meniscus (partial meniscectomy) or a meniscal repair. Newer instrumentation and technology has allowed many of these repairs to be done in a less invasive fashion arthroscopically. Post-operative recovery from a partial meniscectomy can be 4-6 weeks, versus a meniscal repair which can take 4-6 months for the repaired meniscus to heal. The goal in treatment is to try and preserve as much functional meniscal tissue as possible, which can help lower the risk of future knee osteoarthritis.
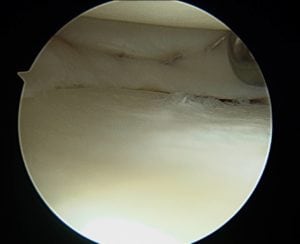
Articular cartilage is the shiny white cartilage that covers the ends of bones where they form a synovial joint. It provides for a smooth gliding surface for the joint to function. Cartilage injuries of the knee refers to the focal loss of articular cartilage in one or more compartments of the knee. Such injuries can be acute or chronic and symptoms may include pain, swelling, locking, or stiffness. MRI imaging is necessary to assess the location and size of the lesion. The size of the defect usually dictates which type of cartilage restoration procedure is necessary. Small chondral defects can be treated with arthroscopic debridement, microfracture, or osteochondral autograft transfer. Large defects require other options such as osteochondral allograft or autologous chondrocyte implantation. If the overall joint alignment is abnormal, an osteotomy or joint alignment procedure may be needed in addition. Recovery from cartilage restoration procedures often requires weightbearing restrictions with crutches for 6 weeks, as well as a formal outpatient therapy program. Overall healing time and full recovery can be up to 4-6 months or longer.
Patellar instability refers to subluxation or dislocation of the patella from the trochlear groove. A number of anatomic factors can predispose a patient to patellar instability. These include baseline ligamentous laxity, a high riding patella (patella alta), or a shallow groove (trochlear dysplasia). Injuries often occur secondary to a traumatic mechanism and the direction of dislocation is typically lateral. An initial subluxation stretches the main stabilizing ligament called the medial patellofemoral ligament. An acute patellar dislocation can also damage the articular cartilage of the patellofemoral joint, which can lead to a loose body within the knee joint. This can necessitate an arthroscopic surgery for loose body removal. An initial subluxation or dislocation event predisposes patients to an increase risk of future patellar instability episodes. In recurrent cases, surgical treatment includes reconstruction of the medial patellofemoral ligament. In cases with more pronounced bony mal-alignment, a bony reconstruction procedure called a tibial tuberosity osteotomy is added to improve stability. Patients use a hinged brace for 6 weeks post-operatively and require a structured physical therapy program. Overall return to sport can be 4-6 months or longer depending on progress with physical therapy.
Osteoarthritis affects over 30 million Americans. It involves the gradual breakdown of joint articular cartilage, which places increased stress on the underlying subchondral bone. The knee can be viewed as having 3 main compartments (medial, lateral, and patellofemoral). The arthritic process may involve one compartment more than the other, or can be more generalized in nature. Risk factors for osteoarthritis include age, gender, race, genetics, prior joint injury, limb malalignment, and obesity. The severity of arthritis can vary significantly from patient to patient. Symptoms include pain, swelling, stiffness, and deformity. Diagnosis includes physical exam and weightbearing x-rays. Various non-operative and operative treatment options exist. Non-surgical options include weight loss, activity modification, quadricep and hip strengthening, corticosteroid injections, viscosupplementation injections, platelet rich plasma injections, and bracing. Surgical options can include osteotomy in younger patients and partial or total joint replacement. Joint replacement procedures can greatly improve one’s quality of life by decreasing pain and improving function of the joint. The surgery usually requires a 2-3 day hospital stay. After discharge, outpatient and/or home therapy exercises are extremely important for gait re-training, knee range of motion, and strength recovery. Full recovery can take 4-6 months in some patients.
