Knee Anatomy and Arthritis
 Osteoarthritis is the most common form of arthritis and affects many people after middle age. It is often referred to a degenerative joint disease. There are many ways to treat arthritis to minimize pain, improve function, and provide quality of life.
Osteoarthritis is the most common form of arthritis and affects many people after middle age. It is often referred to a degenerative joint disease. There are many ways to treat arthritis to minimize pain, improve function, and provide quality of life.
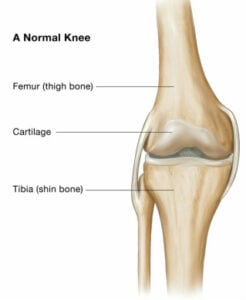
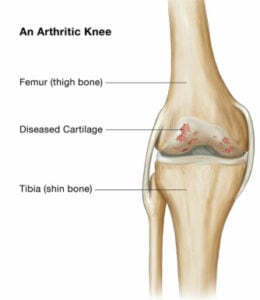
Arthritis affects the cartilage, or smooth lining that covers the surfaces of the knee joint. It is a very low friction interface that allows fluid motion in the normal knee. In the arthritic knee, the cartilage layer degenerates and can wear away, exposing the underlying bone. This may cause “Bone-on-bone Arthritis”. Cysts, or holes in the bone, and bone spurs called osteophytes may develop.
Causes of arthritis can be many. Sometimes previous injury or trauma causes wear. Abnormal alignment and motion can increase wear. Genetics may also play a role – patients with a strong family history of arthritis may be more likely to develop it themselves. In some cases, a condition called avasvcular necrosis can cause significant change and collapse of a joint when part of the bone dies.
 Symptoms of arthritis usually include pain and loss of motion. Pain is the first sign for most patients. It can be associated with stiffness. At first, symptoms may only present with activity. As the disease progresses, patients may experience pain even at rest or at night.
Symptoms of arthritis usually include pain and loss of motion. Pain is the first sign for most patients. It can be associated with stiffness. At first, symptoms may only present with activity. As the disease progresses, patients may experience pain even at rest or at night.
The diagnosis of arthritis is made with a history and physical exam by your doctor. X-rays or other imaging may be performed to determine the extent of the damage and possibly the cause. If infection or other conditions such as Rheumatoid Arthritis are suspected, bloodwork or labs may be required.
Treatment of arthritis can usually begin with simple measures that your primary care physician may begin. These may include physical therapy and weight loss, over-the-counter medications or prescriptions, or assistive devices such as a cane or brace. Oftentimes injections can be helpful for an arthritic joint.
In some cases, surgery may be appropriate and necessary for the treatment of significant arthritis.
Knee Surgery
 Arthroscopy, or a “knee scope” is an outpatient procedure. Through very small incisions, a surgeon can use a camera and small instruments to clean up an arthritic joint, treat or repair tears in a meniscus, repair certain types of cartilage injury, or reconstruct torn ligaments.
Arthroscopy, or a “knee scope” is an outpatient procedure. Through very small incisions, a surgeon can use a camera and small instruments to clean up an arthritic joint, treat or repair tears in a meniscus, repair certain types of cartilage injury, or reconstruct torn ligaments.
Osteotomy is a procedure where the joint is realigned. This can help to redistribute the forces across a joint and ease pain and slow the progression of arthritis. This is also a procedure usually reserved for younger patients and is a fairly large operation with significant recovery time.
Total Knee Replacement is a definitive solution for arthritis of the knee. In this procedure, all parts sides of the joint, the femur, tibia, and patella replaced with components that act just like a normal knee. All arthritic surfaces, and any parts that move on one another are resurfaced. Some patients may be candidates for a less invasive procedure, a partial knee replacement, where only the affected part of the knee is replaced.
 Total knee replacement (TKR) is the most common surgical procedure used to treat a patient with an arthritic knee. It can restore function and relieve pain associated with a significantly affected knee. In total knee replacement, all parts sides of the joint, the femur, tibia, and patella replaced with components that act just like a normal knee. All arthritic surfaces, and any parts that move on one another are resurfaced. Some patients may be candidates for a less invasive procedure, a partial knee replacement, where only the affected part of the knee is replaced.
Total knee replacement (TKR) is the most common surgical procedure used to treat a patient with an arthritic knee. It can restore function and relieve pain associated with a significantly affected knee. In total knee replacement, all parts sides of the joint, the femur, tibia, and patella replaced with components that act just like a normal knee. All arthritic surfaces, and any parts that move on one another are resurfaced. Some patients may be candidates for a less invasive procedure, a partial knee replacement, where only the affected part of the knee is replaced.
While most patients who undergo total knee replacement are between ages 55 to 80, indications for surgery include both younger and older patients, depending on their pain and disability. People who need knee replacement surgery usually have problems walking, climbing stairs, and getting in and out of chairs. They may also experience moderate or severe knee pain at rest.
Recommendations for surgery are based on a patient’s pain and disability, not age. Total knee replacements have been successfully performed at all ages, from the teenager with juvenile arthritis to the elderly patient with degenerative arthritis.
In most cases, a total knee replacement becomes the best option when your arthritic knee causes so much pain that it interferes with your overall quality of life. For many patients, this means that the arthritis pain limits walking, standing, climbing stairs, or interferes with sleep.
During knee replacement, a surgeon cuts away damaged bone and cartilage from your thighbone (femur), shinbone (tibia) and kneecap (patella) and replaces it with an artificial joint made of metal alloys and high-grade plastics.
One of the more recent advances in knee replacement surgery is the unicompartmental knee replacement (also known as a unicondylar knee replacement). This type of knee replacement is less invasive than a full knee replacement.
The operation is designed to replace only the portions of the joint that are most damaged by arthritis. This can have significant advantages, especially in younger patients who may need to have a second artificial knee replacement as the first one begins to wear out. Removing less bone during the initial operation makes it much easier to perform a revision artificial knee replacement later in life.
Many patients note that recovery from a partial knee replacement is easier than a total knee. It also may feel more like a natural knee because the major ligaments which are routinely removed in total knee replacement are retained.
Cementless Partial Knee Replacements
 Further advances in materials, manufacturing and technology innovation, have given rise to the cementless Partial Knee Replacement. The advantage of a cementless approach is the implants include porous surfaces that mimic human bone, and as a result can take advantage of the natural healing properties to create reliable implant fixation. This biological fixation strategy is less susceptible to deterioration over time than traditional implants that rely on bone cement. In addition to this, eliminating cement from the surgical procedure allow for reduced time in the operating room and reduced time under anesthesia.
Further advances in materials, manufacturing and technology innovation, have given rise to the cementless Partial Knee Replacement. The advantage of a cementless approach is the implants include porous surfaces that mimic human bone, and as a result can take advantage of the natural healing properties to create reliable implant fixation. This biological fixation strategy is less susceptible to deterioration over time than traditional implants that rely on bone cement. In addition to this, eliminating cement from the surgical procedure allow for reduced time in the operating room and reduced time under anesthesia.
Dr. Harris is proud to be one of the first surgeons in the country to offer his patients the
first cementless Partial Knee Replacement available in the US optimized for treating
medial compartment disease.
This unique implant, called the Engage Partial Knee System, has been optimized for
outpatient surgery.
Custom knee replacement is a new technology in total knee replacement. Rather than using traditional jigs and guides for performing the surgery, the guides are custom-made to fit an individual patient’s unique anatomy. All of the planning is done before surgery based on a CT or MRI scan of your knee. A 3-D computer model is generated. This allows for very precise detail and precision in implant placement and alignment.
Custom cutting guides are then made based upon the surgical plan and computer model. Each pair of guides is unique and matched to one patient, one knee. The result is a more efficient surgical process with predictable results.
While not every knee replacement requires custom guides, they can offer specific advantages in many patients.
